Scroll through social media and you’re bound to come across a handful of “what I ate this week” reels, showcasing absurdly neat, insanely colourful plates of food. I’m sure I’m not the only one to scoff at these posts, and wonder who subsists only on smoothies for lunch or whips up grain-free pancakes every morning. We all know, on some level, that these representations aren’t a true reflection of how most people eat. What’s more, many posts focus less on health and more on weight loss as their primary goal.
(Related: A Dietitian Helps Us Debunk the Outdated Myths About MSG)
Melissa Fernandez, an assistant professor at the University of Ottawa’s School of Nutrition Sciences, says that nutrition influencers in particular play a big role in popularizing fad diets. “It’s because of how easy it is on social media platforms to visually communicate these plans, foods, trends and ideologies,” explains Fernandez. Compared to a cookbook or a daytime TV segment, which is how diets were often pushed in the past, content on social media appears so much more immediate—and visceral. Social media algorithms create an echo chamber of diet trends—click on one and you’ll be continuously fed new but similar posts. “That reinforces the value of these diets,” says Fernandez, “because you keep on seeing the same messages portrayed in similar ways.”
Fernandez points out that anecdotal evidence—sharing personal experiences with diets—is also a powerful tactic harnessed by influencers because it makes them more relatable to their followers. The diets they push are often conveyed as simple solutions with quick results. “They bring in words like well-being and mental health to make it sound more holistic,” says Fernandez. “But at their core, these eating plans are still either low-calorie, low-carb or low-fat.”
Nutrition influencers aren’t necessarily medical professionals. “Consumers need to be very critical about what comes up first on their feeds,” Fernandez says. “The large majority of nutrition influencers don’t have any actual expertise in nutrition.” And their credentials can be misleading. “Consumers assume that a holistic nutritionist is a legitimate title, but anyone could take an online course and become a holistic nutritionist,” she explains. “They are not licensed health-care professionals.” As a first line of defence against nutrition misinformation, look to medical doctors, registered dieticians, pharmacists and nurse practitioners for advice on health, and healthy eating.
Nutrition influencers are entrepreneurs, so they’re going to promote ideologies around food that will help build their audience. Fernandez says this often leads to catchy, clickbait-y and sometimes controversial or misleading messaging appearing front and centre because it means more clicks and more followers. They may also promote products and services as part of a paid partnership, which isn’t always obvious.
It can be hard to discern who to trust and follow in the online food space, especially when not everyone with a large platform is credible. But you can look for red flags. We asked Fernandez, along with two registered dietitians, Acacia Puddester from Acadia University and Erin O’Flaherty from St. Joseph’s Healthcare Hamilton, to explain social media’s most popular diet trends, and why you should be skeptical of anyone who promotes these eating plans.

Intermittent fasting
Intermittent fasting involves eating during a designated period and abstaining from any food or drink for the rest of the day. For example, someone might consume all their meals during a six-hour window, and fast for the remaining 18 hours. What makes this diet appealing is that it restricts the period of time that food can be consumed, not the quantity or type of food. But O’Flaherty says that there’s a gender difference in how we respond to intermittent fasting. Women’s bodies respond more quickly to food deprivation, releasing more of the hunger hormone ghrelin and decreasing levels of our satiety hormone leptin, all of which can make it harder to stick to a strict eating schedule, compared to men. In addition to those two hormonal changes, the body will also release a neuropeptide Y that stimulates the want for food intake, specifically carbs for quick energy—your body thinks you’re starving and goes in search of quick energy.
Fasting also affects women’s hormones differently. “When women are intermittent fasting, our metabolism slows down and the stress in our bodies increases, which affects our hormonal health negatively,” O’Flaherty explains. “We’re slowing down to conserve energy.” She says that this, in turn, may affect fertility: “We’re telling our bodies that this is not a good time to make children.” Being hungry keeps us in a heightened state—our body is urging us to find food right away.
Equally detrimental, according to O’Flaherty, are the mental health impacts of intermittent fasting. “It can increase the risk of disordered eating because we’re relying on external cues to tell us when to eat instead of checking in and being intuitive about our hunger or fullness, how much we need to eat and when we need to eat,” she explains. “We’re breaking down that trust between our body and ourselves.”
Leaky gut
Gut health has been a buzzy subject lately, for good reason. New research and data show a strong connection between our gut and our mental health, skin health, immune system and more. But “leaky gut syndrome” in particular is an invented condition that claims symptoms like diarrhea, bloating and fatigue are caused by bacteria and toxins “leaking out” of the intestinal lining. It’s something that Puddester is desperate to debunk. “Leaky gut syndrome is not a medical term,” she says. “It’s not a medical diagnosis. It is made up.”
Puddester says the term has been promoted by alternative health professionals without nutritional or medical backgrounds. She believes it has caught on partly due to self-transformation content on TikTok and Instagram, and the popularity of “before and after” posts populated with bloated belly images. Fear-mongering plays a role, too. “‘Leaky’ sounds like something that shouldn’t happen,” Puddester says. But, in fact, that’s how a healthy digestive system works—it’s completely normal for your body to absorb nutrients like proteins, fats, vitamins, minerals and water through the small intestine.
The symptoms of so-called leaky gut syndrome are pretty common, which is also what drives its online popularity. “When people experience these gastro symptoms, and they google them, they see this leaky gut ‘diagnosis,’” Puddester explains. However, gastrointestinal issues should always be discussed with a dietician or medical professional. “It could be the result of celiac disease, irritable bowel syndrome, an e.coli infection or many other factors,” she says. Some women experience gastro discomfort during the luteal phase of menstruation, others are particularly sensitive to certain foods, like cruciferous veggies (think broccoli, Brussels sprouts and cauliflower).

Whole30
This 30-day diet cuts out added sugar, alcohol, dairy, dairy, grains, legumes and additives like sulfites (a preservative) and carrageenan (used to thicken food). Fernandez acknowledges that reducing the consumption of sugar and alcohol has health benefits. But eliminating entire food groups, like legumes and dairy, is a red flag. “It has the potential to create nutritional deficiencies,” she explains. “Legumes are a healthy food!”
Following a Whole30 eating plan might result in weight loss after a month, but Fernandez cautions that the results are short-term. “There’s a lot of weight regain after the diet is over,” she says. “To avoid that, you have to maintain the diet, which is hard to keep up long-term.” Fernandez advises following a healthy, flexible and balanced meal pattern instead, like the Canadian or American food guide, or the Mediterranean diet, which encourages eating fruits, vegetables, whole grains, fish, poultry, beans, nuts and vegetable oils while limiting (but not eliminating) high saturated-fat foods like fatty meats, full-fat dairy, sugary drinks and sweets.
Detoxes, cleanses and resets
These diets, which replace meals with vegetable and fruit juices and sometimes proprietary supplements, are marketed as helping your digestive tract absorb nutrients. They might make people feel better in the short term, since they cut out refined sugar and the processed foods that can make us feel bloated. But Fernandez warns that juice cleanses, for example, are really just low-calorie diets in disguise. “They might give you 600 calories a day, as opposed to the typical 2,000, for example,” Fernandez says. So if you’re doing that for a week, you’re going to lose weight because you’re simply not getting enough calories.”
Fernandez also encourages us to be critical of any messaging around cleansing toxins from our bodies. “The word ‘toxin’ is used to scare people,” she says. “It attracts viewers and followers, but it doesn’t really mean a lot. There are toxins all around us. There are toxins that are natural in the foods that we eat.” And in fact, our livers, kidneys, bladders and skin already do an excellent job at removing them.
Laxative-based cleanses are also a red flag for Fernandez. “If you’re not suffering from constipation, there’s no reason to take a laxative,” she says. “You’re likely dehydrating yourself, and it can have negative impacts on bone health.” While some cleanses may claim to be beneficial for gut health, Fernandez says that the opposite is true. “It can really disrupt your gut microbiota,” she says. “If you’re eliminating bacteria from your gut, you’re eliminating the good and the bad.”
FODMAP
Fernandez says that the FODMAP diet, which reduces or limits foods that are high in fermentable carbohydrates such as honey, mango, garlic, beans and dairy, does serve a medical purpose. “It’s a therapeutic diet for people who have [diagnosed] irritable bowel syndrome,” she says. “It’s quite effective to reduce some symptoms related to IBS and improve patients’ quality of life.” However, Fernandez says, the diet is highly individualized for each person that goes on it: “It’s usually something that’s done under the care of a health-care provider like a dietitian or a doctor.” Going rogue and doing a FODMAP diet on your own to cure gastrointestinal issues can exacerbate the underlying problem. “Eliminating foods can result in nutritional deficiencies,” Fernandez says. Plus, it’s highly personal as to which items trigger your IBS. First step: talk to your doctor.

Keto
The goal of this high-fat, low-carb, moderate-protein diet is to put your body into a state of ketosis, where you break down fat instead of carbs for energy. “Our bodies use carbohydrates for energy, so if we don’t have carbohydrates coming in, then our body has to break down something else,” explains O’Flaherty. The idea of forcing your body to burn fat makes the keto diet sound alluring. “The problem is that ketosis is actually a starvation response,” she says. “It can be dangerous because it changes the acidity of our blood.” Another issue is the keto diet’s high-fat requirement. “Not all fats are created equal,” O’Flaherty says. “I’ve seen a lot of people increase their cholesterol levels and worsen their heart health following keto eating plans.” The diet was originally developed in the 1920s as a treatment for refractory epilepsy (fasting appeared to reduce the incidence of seizures). But it has become so popular in the last decade that keto-specific restaurants have popped up in Toronto, Calgary and Vancouver, and grocery stores stock keto-friendly versions of foods like pizza crusts and burger buns.
No Sugar
Like Fernandez, Puddester cautions against any diet or ideology that eliminates an entire food group or ingredient. “Sugar is not bad,” she says. “It’s essential to give us the glucose that our bodies, and especially our brains, need.” While reducing excessive amounts of sugar can be beneficial for your health, there’s no need to banish it. “Fruits are quite high in sugar, but they’re also high in a lot of other nutrients, like vitamins, minerals and fibre,” she says. “And we certainly don’t want to cut those out if they can offer us good health benefits, which they do.”
A common refrain of no-sugar dieters is talk of being “addicted to sugar.” But Puddester is quick to dispel this myth. “There’s no scientific evidence to show that any food is addictive,” she says. The feeling of craving something sweet isn’t the same as being addicted to a drug. Really, eliminating any food can result in cravings, according to Puddester. “Our bodies will crave because there’s a psychological impact: We all want what we can’t have.” Often, she says, our cravings tell us what we’re missing. “I think it’s those cravings that make people think, ‘I’m addicted,’” explains Puddester. “But it’s not an addiction. It’s your body asking you to not be so restrictive.”
Fernandez acknowledges that part of what makes any of these diets enticing is that they offer a framework for meal plans, which helps with the burden of meal prep: deciding what to buy, shopping, storing ingredients and cooking. “That’s often the hardest part about eating healthy,” she says. Having a community support group can help sustain your motivation to choose those whole grains, healthy fats, fruits and veg—but that community doesn’t have to be centred on a restrictive diet. Instead, try to connect and share inspiration with friends who enjoy food, and trust your body’s cues.
Next: Do Healthy Chips Exist? A Dietitian Weighs In on Our Favourite “Healthy” Snacks
There’s a whole lot more MNRA can do
Messenger RNA, or mRNA, are like microscopic blueprints for the body. They show our cells how to assemble an important protein—like, for example, COVID’s infamous spike—so our body recognizes that protein as something foreign and dangerous, and mounts an immune response. mRNA vaccines are safe, effective and lightning-fast to produce: “As long as we know the protein to encode, we can do it in the lab in about two weeks,” says Anna Blakney, an assistant professor at the School of Biomedical Engineering and the Michael Smith Laboratories at UBC. “Now that we have these mRNA vaccines for COVID, we’re thinking about where to go next.”
The mRNA platform has massive potential for cancer treatment. Cancer is a far more complex disease than COVID; there’s no single target, like the spike, to protect the whole population against. But the speed and precision of mRNA sequencing opens up the possibility of personalized medicine: You take a biopsy from a patient’s tumour, see what proteins are specific to that tumour and design a purpose-built vaccine. “That’s huge, because it means we may not have to use chemotherapy and drugs that are very non-specific and have really high side effects,” Blakney says.
In her lab, Blakney and her team are working on a vaccine for chlamydia, a disease that can cause pelvic inflammatory disorder and lead to infertility in women. “We really need a vaccine to prevent it, similar to the HPV vaccine,” she says. Their ovarian cancer project is trying to encode an antibody called a bispecific T-cell engager—or BiTE—that helps T cells kill cancer cells. And their work with Toronto’s Sunnybrook Hospital will see if RNA can reprogram cells into neurons to change the progression of neurodegenerative disorders like Alzheimer’s. “This was not something I was thinking about even five years ago,” Blakney says. “The breadth of the applications is what’s so exciting.”
Your pelvic floor deserves a custom fit
and that’s very much not the case for women who may experience prolapse (up to 50 percent of us!). Right now, treatment comes down to surgery or an off-the-shelf pessary, but Toronto-based Cosm uses AI and 3D printing for a personalized pessary, a big improvement on a design that has not budged in 50 years.

Stem cells could give us back our sight
The eye is a finicky organ, and once our retinal cells are damaged from diseases like glaucoma, those cells are gone for good. At UHN’s Donald K. Johnson Eye Institute, postdoctoral researcher Tahani Baakdhah takes pluripotent stem cells—which can be nudged to form any sort of cell in the body—and encourages them to transform into retinal ganglion cells, the neurons that connect our eyes to our brains. “We’re moving toward transplanting these cells into animal models and seeing if they can make that connection,” Baakdhah says. The work isn’t easy; it’s going to take some time. “But I’m having good vibes about this,” she says. “I’m optimistic I will help people see this beautiful, colourful world.”
Bioprinted mini brains will map dementia
For decades, scientists have been on the lookout for effective treatments for neurodegenerative disease, to no avail. So researchers at the University of British Columbia decided to take matters into their own hands, combining stem cells from the blood of Alzheimer’s patients with a state-of-the-art 3D bioprinter in order to grow pint-sized tissue models of the patients’ very own brains. With these mini models, researchers are able to study the disease’s progression, see how the brain tissue reacts to treatments and, ultimately, discover new drugs that could slow or even halt the march of dementia.
We’re finally collecting better data…
Until just a few years ago, we knew way more about the rat brain than the female human brain. “It’s a very humbling starting point,” says Esther Bui, a neurologist and epilepsy specialist at UHN’s Krembil Brain Institute. “There’s so much work to be done.”
Before 2021—when it became required, where appropriate, to include sex and gender in research projects—80 percent of human neuroscience research did not consider sex as a biological variable. Bui breaks it down: “Women were systematically excluded from clinical trials because it was ‘too complicated’ to track periods, or it was too worrisome to include women who may become pregnant. And yet it’s not too complicated to map out the whole genome sequence?” We should all feel so incredulous. Women’s symptoms of diseases, common or life threatening, are often called atypical but atypical only because most diseases have been heavily studied in men. It means women have a higher chance of being misdiagnosed or dismissed by their healthcare provider.
Happily, Bui says this is a “supernova” time for women’s neurology, where research and education are
finally catching up—in 2019, she developed Canada’s first accredited Women’s Neurology Fellowship training—and we can better define precision medicine for women. “Everyone tells me what I’m not doing is not visionary work,” Bui says. “But visionary work is not just looking forward. It’s also looking back to make sure no one is left behind.”
… And that data will be inclusive
Janet Tootoosis is trying to understand what health progress looks like from an Indigenous perspective. As the vice dean of the Division of Indigenous Health at the University of Saskatchewan’s College of Medicine, she is committed to a strength-based approach, which empowers both patients and practitioners by moving the focus away from health deficits and toward Indigenous people’s capacities and capabilities. The new department—the first of its kind in Canada—aims to integrate Indigenous teachings with western medicine, give physicians opportunities to enhance their skills in Indigenous health and provide Indigenous med students the option of having specialized credentials. Tootoosis insists that the people who’ve been failed by our current health-care system—and by academia—must form the inner workings of the new department. And she’ll measure success by the impact she makes at the community level. “I want Indigenous people to say: I like what you’re doing at the College of Medicine.”
The smallest molecules will have a big impact on diagnosis
Over the course of our lifetimes, we’re exposed to all manner of tiny molecules. Some of them come from our world, in foods or shampoo. Some of them are in our bodies, like sugars and fats. Together, they give researchers a picture of how our genes interact with the environment, especially when it comes to what might trigger disease.
That’s handy, because many diseases rely on clinical diagnosis, which determines a disorder based on a patient’s symptoms. “But something like pain is quite subjective,” says Nikita Looby, PhD, a scientific associate at UHN’s Schroeder Arthritis Institute. The goal of metabolomics—the study of these molecules, called metabolites—is to move to objective measures in order to diagnose diseases, monitor their progression and evaluate the response to treatment.
Looby’s work focuses on psoriatic arthritis, which can lead to irreversible damage and disability. “There are so many ways in which this disease can manifest that make it difficult to nail down,” Looby says. “It drives me insane, to be honest.” She wants to take all those patient symptoms and correlate them with the presence and concentration of different metabolites. “Then we can run a rapid test on someone’s blood sample and, based on the metabolites, know what the diagnosis is and figure out the treatment.”
But metabolomics could allow researchers to be proactive, as well. When we know what molecular markers are associated with arthritis—or any sort of disease—we can develop drugs to intervene before the damage is done. “The entire idea behind metabolomics,” Looby says, “is that one size doesn’t fit all, and one drug doesn’t solve all.”
There’s new hope for preemies
Incubators can only do so much. At Toronto’s SickKids hospital, researchers are investigating artificial placentas that could deliver essential oxygen and nutrients to preemies and let doctors more safely perform life-saving surgeries.
We can wrangle syphilis back into submission
Syphilis rates have skyrocketed in recent years, especially among women of child-bearing age: Between 2016 and 2020, cases went up a whopping 775 percent, according to the Public Health Agency of Canada. But diagnosis and treatment can be a challenge—people might be reluctant to access health care services, or they don’t return once their blood has been taken. That’s why University of Alberta infectious disease expert Ameeta Singh helped research a rapid test that identifies syphilis and HIV in a flash, so people can be tested and treated in a single visit. “It also works really well in a variety of settings, whether that’s on the street, in a van or in community health centres,” she says.
Breast milk will help everyone—not just newborns
Breast milk has major benefits for immunocompromised folks, so biotech company Lactiga is making it into medicine. Taken via pills or an inhaler, it gives
immunocompromised people a boost in their fight against COVID, mucosal diseases and gastrointestinal infections.
Drones will drop medicine where you need it
Rural, remote and Indigenous communities often struggle to provide health care to the people who need it—medical supplies take too long to get there, if they can get there at all. When resources can’t get to patients, patients have to be brought to resources, which costs precious time. So family doctor John Pawlovich is working with the University of British Columbia to see how drones can help out. Over the course of a year, one small drone, packing prescriptions and other medicines, carried out 1,200 flights in all conditions between Stellat’en First Nation and the Village of Fraser Lake. Next up: testing bigger drones that can travel longer distances (and even up over mountains) to make remote health care more accessible—and more equitable.

A trusty home blood-pressure monitor adds years to our lives
Let’s start with some uncomfortable facts. More than 108,000 Canadians experience a stroke each year, a statistic that has nearly doubled over the past two decades. Stroke kills twice as many women annually as breast cancer, and among people under 55, rates are on the rise, due in part to lifestyle-related risk factors like sedentary behaviour, substance use and stress. Still, studies show that 70 percent of women don’t know about any of the stroke risk factors. It’s a statistic that worries neurologist Aleksandra Pikula, research director of UHN’s Stroke Program, and one she’s hoping to change in her capacity as the inaugural Jay and Sari Sonshine Chair in Stroke Prevention and Cerebrovascular Brain Health at UHN’s Krembil Brain Institute.
The biggest culprit for stroke is high blood pressure, which often ticks up during perimenopause. “I have a truly powerful message for all women approaching midlife,” Pikula says. “Know your numbers.” Normal blood pressure is below 120 over 80. Anything higher and you should be checked by your primary care provider—and you must start working on lifestyle changes. With just a five-point decrease in blood pressure, our risk of stroke can drop by up to 20 percent, so start small: Cut back a little on salt or ultraprocessed foods. Maybe walk 10 or 15 minutes a day. Eighty to 90 percent of strokes are linked to modifiable risk factors, says Pikula, and when she says modifiable, she means we can work on them.
High blood pressure is a silent killer. It doesn’t hurt and there are no symptoms until it is severely high, but it can wreak havoc on your cardiovascular and brain health. A home blood pressure monitor is a basic tool that delivers vital information, and any adjustments you make to your lifestyle—in terms of nutrition, physical activity, sleep, stress, social connections and substance use—will pay big dividends in your overall health. As Pikula points out, “what works for the prevention of diabetes works for the prevention of cardiovascular conditions works for prevention of stroke.”
A breath test could detect lung cancer
The deadliest form of cancer, with rates that are only going up in non-smoking women. At the BC Cancer Research Institute’s Breathomics Lab, researchers catalogue thousands of biomarkers in hundreds of breath samples to build a non-invasive breathalyzer test that can catch lung cancer early.
We’re trying to get to the bottom of pain
The medical community is fuzzy on pain. It can be hard to establish severity— everyone’s “five” on a pain scale is different—and in the absence of an objective test to determine treatment, discrimination creeps in. Although roughly half of all chronic pain conditions are more common for women, doctors are more likely to dismiss their pain. Here’s just one example: Middle aged women with symptoms for heart disease (like chest pain) are twice as likely to be told the cause is mental illness than men with the same symptoms, whose conditions are taken more seriously. Mojgan Hodaie, a neurosurgeon at Toronto Western Hospital, is on a quest to better understand where in the brain pain comes from, what consequences it has, and how to make sure it’s given its due. “Doctors have all sorts of unconscious biases,” Hodaie says. “How can we take pain from being a purely subjective phenomenon to one with a greater objective understanding?”
By coupling machine learning with brain images, her team created a brainage calculator that looks at the gap between how old a person’s brain appears and their actual age. Women, they found, are most at risk for accelerated brain aging across more types of chronic pain. Why does this happen? That’s also what Hodaie is trying to find out, in order to unlock more targeted treatments—ones that really consider the snowball effects of chronic pain, rather than just bandage over them.

We can make a better blood vessel
When you get sick, or are diagnosed with a chronic condition, it’s often because cells in your body aren’t performing as they should. To restore function, doctors can transplant new cells to compensate for failing ones—but the trick is getting those cells to survive once they’re in your body. New cells die for all sorts of reasons, but a main one is the lack of blood vessels bringing life-sustaining oxygen and nutrients to the transplanted cell. Sara Vasconcelos, a researcher at UHN’s Toronto General Hospital Research Institute and the John Kitson McIvor Endowed Chair in Diabetes Research, thinks artificial blood vessels could be the solution. By growing those vessels in a lab, doctors will be able to transplant them together with the new cells to ensure better compatibility.
Right now, Vasconcelos and her team are working on a few approaches. One involves a form of what Vasconcelos calls “recycling blood vessels,” taking those vessels from parts of the body that can spare them (like fat) and transplanting them into new cells. But sometimes, recycled vessels are also affected by diseases like diabetes, so Vasconcelos is making new small blood vessels from scratch using stem cells. The hope, says Vasconcelos, is to be able to replenish cells wherever they’re failing due to chronic conditions: “This work could be applied to many places throughout the body.”
More doctors will diagnose endometriosis on the spot
At least one in 10 women suffer from endometriosis, but there’s plenty we don’t know about this disease: what causes it, what could prevent it and what a cure might look like. Even diagnosis can be a bit of a crapshoot, based on a set of symptoms or through laparoscopy, a surgical procedure that might take years to get on the books. At McMaster University in Hamilton, Ont., gynecologic surgeon and sonologist Mathew Leonardi has uncovered a far more efficient approach. Trans-vaginal ultrasounds can identify endometriosis—it’s right there in the imaging, if you know where to look. He’s now teaching that skill to practitioners, so more patients can access this minimally invasive diagnostic tool.
“Endometriosis is an invisible disease,” he says, but an imaging test reveals what exactly is happening in our bodies. “It gives us so much more information to guide patients to the right treatment strategies.”
Every recipe I create for my books reflects a facet of how I like to eat in real life. I cannot write a cookbook without an eggplant recipe (or two!) because I love this vegetable so much. I will happily gobble up all four servings of this eggplant—roasted until its flesh is creamy, sprinkled with citrusy sumac and fresh mint, and drizzled with maple syrup–spiked tahini—with zero complaints.
Sumac-Roasted Eggplant with Maple Tahini Drizzle
Serves 4
Ingredients
Main
- 4 Chinese eggplants
- 2 tablespoons (30 mL) avocado oil
- 1¼ teaspoons (6 mL) ground sumac, plus more for serving
- ½ teaspoon (2 mL) salt Freshly cracked black pepper
For the maple tahini drizzle
- 2 tablespoons (30 mL) tahini
- 1 tablespoon (15 mL) pure maple syrup
- 1 tablespoon (15 mL) water
- ⅛ teaspoon (0.5 mL) salt
For serving
- Flaky sea salt
- 1⁄3 cup (75 mL) packed fresh mint leaves, thinly sliced
Instructions
- Roast the eggplant: Preheat the oven to 400°F (200°C). Line a baking sheet with parchment paper.
- Cut the eggplants in half lengthwise. Using a paring knife, score the halves diagonally, spaced ½ inch (1 cm) apart. Place the eggplant cut side up on the prepared baking sheet.
- Brush the eggplant with the avocado oil. Sprinkle with the sumac, salt, and lots of pepper. Turn the eggplant halves over so they are cut side down on the baking sheet. Transfer to the oven and roast until soft and golden brown on the cut side, about 45 minutes.
- Meanwhile, make the maple tahini drizzle: In a small bowl, whisk together the tahini, maple syrup, water, and salt.
- To serve, pile the eggplant on a serving platter. Spoon the maple tahini drizzle over the eggplant. Sprinkle with a bit more sumac, flaky sea salt, and mint. Store leftovers in an airtight container in the fridge for up to 2 days. (I like to chop and fry the leftover eggplant, then add a bit of water and any leftover maple tahini drizzle until warmed through.)
Excerpted from Plant Magic by Desiree Nielsen. Copyright © 2024 Desiree Nielsen. Published by Penguin, an imprint of Penguin Canada, a division of Penguin Random House Canada Limited. Reproduced by arrangement with the Publisher. All rights reserved.
Next: A Gluten-Free Carrot Cake That Tastes Like the Real Deal
Leonardo DiCaprio is obsessed with it. LeBron James bought a team. Grand Slam tennis champ Serena Williams said she could make it her second career. And, recently, my friends and I also picked up this buzzy racquet sport.
Pickleball is the fastest-growing sport in North America, boasting nearly 5 million players on this continent with millions more worldwide. From 2020 to 2022, the number of participants in Canada tripled, with about one million “picklers” playing monthly. Although older adults were the early adopters, today the largest increase is among millennials, with female participants outnumbering men in most age groups.
The sport is an amalgam of badminton, table tennis and tennis. Just swap a tennis racquet for a smaller, solid-faced paddle and the fuzzy ball for a plastic Wiffle ball, set the net eight inches lower, shrink the court down to about a quarter of its size and you’ve got the makings of a pickleball game. The condensed playing field makes it less taxing on the body and allows for more rallies—and chit-chat. For first-timers, these differences make the sport more welcoming and easier to pick up.
Pickleball might seem like it arrived to enthusiastic fanfare overnight. However, its inception can be traced back to the summer of 1965, when three American dads concocted the game while trying to entertain their bored kids. More recently, it surged in popularity during the pandemic lockdown, when many people were looking for new outdoor activities to help them safely stay fit. Pickleball has now made the leap from backyard pastime to primetime, with televised matches and celebrity tournaments.
Drummond Munro, a lifelong racquet-sports enthusiast, was introduced to pickleball in South Carolina six years ago. This past summer, he co-founded Fairgrounds Public Racket Club, a public pickleball court in Toronto, and has plans to roll out more locations across Canada. Munro’s goal is to introduce the sport more widely and democratize the culture around sports clubs. “We’re building a new type of social club that removes that elitist, exclusive nature often associated with traditional clubs,” says Munro. While many sports clubs have invitation-only admittance and high initiation fees, plus yearly dues and minimum spends, Fairgrounds is accessible to all ages—anyone can book a court time online—and inexpensive ($10 per visit, with free admission on Tuesdays).
Catherine Parenteau, 27, is a Montreal native and the number two-ranked international pro pickleball player. She picked up the sport seven years ago after being sidelined from competing in tennis once her full scholarship at Michigan State University ended. Since she began touring as a pro pickleball player, she’s witnessed the sport explode worldwide. “It’s much easier than other [racquet] sports to get a rally going because the ball doesn’t bounce as much. This allows you to control your shots more and keep the ball going,” says Parenteau. She also likes that the sport is inclusive and crosses all generations and abilities. “I can hit balls with my grandmother and have great rallies. You can play with someone of any age and level.”
The initial draw for my own group of friends was the social aspect that allowed us to participate in an event together. That we could learn a new sport while engaging in an athletic activity outdoors was simply a bonus. Pickleball strikes the perfect balance of fun and fitness. Plus, it’s beginner-friendly, which makes it easy for newcomers to join our pick-up matches. Our rotating roster of friends and family balloons every week—it even brought out our Gen Z offspring. By 2030, pickleball is projected to have 40 million people playing worldwide, and our kids and parents will likely be included among those fans.

The health benefits of pickleball
Here are all the ways this racquet sport is a smash hit for your body and mind.
Heart Health
Pickleball combines short bursts of intensity with periods of recovery, which is a great way to condition the heart and strengthen your cardiovascular system, says registered physiotherapist Meg MacPherson.
Muscle Control and Strength
“Our bodies are designed to move—and to move in various directions. These sudden multidirectional movements improve muscle control. Over the course of a match, you’ll engage nearly every muscle from the upper body to your legs and core,” says MacPherson.
Cardio Boost
You can expect a heart-pumping workout during an hour-long match. According to researchers at the University of Manitoba, people playing singles or doubles can clock heart rates that indicate moderate to vigorous activity. Apple recently added pickleball to its roster of trackable workouts; on average, you can burn 400 to 700 calories per hour.
Agility
With its sudden movements and lower downtime, pickleball encourages agility and a higher control of your actions, says MacPherson. That allows you to react swiftly and effectively to your environment.
Social Connection
MacPherson notes that participating in a sport that allows you to engage with others can release endorphins (those feel-good brain chemicals that also work as a natural painkiller).
Coordination
Racquet sports famously improve hand-eye coordination, a skill essential for initiating and reacting to action.
Up Your Game
Three expert tips from Catherine Parenteau:
- Always try to return the ball deep (meaning close to the opponent’s baseline) so you have time to set up your next shot.
- Ensure the ball’s contact point is in front of your body for maximum control of your shot.
- Don’t be afraid of the “kitchen”—a zone that extends seven feet from the net on both sides. While you can’t enter the kitchen if the ball hasn’t already bounced, you can still reach in to hit it as long as you keep your feet behind the kitchen line.
Next: This Yogi Will Make You Want to Take Up Surfing
Milan Frydrysek never worried much about his health. His wife worried enough for both of them. Her brother was diagnosed with pancreatic cancer at age 62 and died a little more than a year later. After that, she wanted to do everything possible to stop cancer from grabbing hold of anybody else she loved.
The Frydryseks heard about Prenuvo, a company that offered diagnostic body scans using magnetic resonance imaging (MRI). For $2,500 per person, they could get a head-to-ankle scan that would pick up solid tumours and 400 other medical conditions, according to the company. Their family physician didn’t love the idea, telling them the scan would likely find things that didn’t matter to their physical health but would make them anxious. The Frydryseks thought the scan might give them peace of mind. In February 2021, they each underwent a one-hour MRI at Prenuvo’s clinic in Vancouver’s South Granville neighbourhood.
Within the week, a 35-page report summarizing the results arrived in their inbox. It broke down the findings by body system and into colours: green meant good, yellow was something to watch and red was urgent. In Milan’s report, under the urinary system section, red letters jumped off the screen. The MRI had picked up a 6.6-by-6.5-centimetre mass on his lower left kidney, “which is suspicious for renal cell carcinoma.”
Frydrysek, who was 69 at the time, contacted his family doctor, who’d also received a copy of the report. The doctor quickly connected him with a urologist. Ten weeks after his scan, Frydrysek underwent surgery to remove his kidney. Pathology confirmed the mass was cancer, but there was no evidence of disease remaining in his body after the operation. “Maybe the tumour was growing my whole life,” he says. “Maybe it would have grown for another 30 years without doing anything. Maybe I would have been gone already. All I can say is, thanks Prenuvo.”
Whole-body MRIs, like those offered by Prenuvo, are now growing in popularity, urged along by a swell of marketing from influencers and celebrities and stories like Milan Frydrysek’s. But this boom in the body-scanning industry is taking place over widespread criticism from many doctors and medical organizations. In the United States, the American College of Radiology issued a statement in April 2023 saying there is no evidence that whole-body screening is beneficial. Health Canada says that “whole-body screening poses a number of health risks and offers no proven health benefits.”
Unlike the targeted MRIs ordered by physicians to investigate a specific health concern, whole-body MRIs are designed to satisfy a person’s curiosity about what’s inside their bodies. There is no physician referral required; just an ability to pay the $2,000 and up fee. These scans pick up lumps and bumps hidden under the skin—things that might be cancer, but might also be entirely innocuous and would never affect a person’s health. The catch: An MRI cannot distinguish with 100 percent confidence whether a finding is harmless or not. A person who receives an unusual finding gets directed back to their regular health team—now, with questions and fears about things that need more investigation in a health system that is already beyond capacity.
Canadians worry that, when something is wrong, they will struggle to access appropriate care quickly in the public health system. More than one in five people in this country do not have access to primary care—that’s six and a half million without a regular doctor or nurse practitioner to turn to when they need help. They face long waits to access potentially life-saving diagnostic imaging. Before the pandemic, Canadians waited an average of 50 to 82 days for CT scans and up to 89 days for MRI imaging, even though the recommendation is 30 days. Against this backdrop, more Canadians are turning to private MRI clinics for medically indicated scans. Private MRIs, first offered in Alberta in 1993, are now available in most Canadians provinces.
Where private whole-body MRIs differ is that they’re sold to people without a clear medical indi-cation—the latest trend in a new era of personal empowerment in health, one where tech sells the promise of optimized wellness through devices like fitness trackers, heart rate monitors and continuous glucose monitoring. In 2010, Rajpaul Attari-wala, a radiologist and biomedical engineer in Vancouver, developed a new MRI machine that could enable privately paid full-body screening. Slowly, his business grew, finding fertile territory in a country where people worried about wait lists for medically necessary MRIs. Now, people were coming to Vancouver from across Canada and even abroad for whole-body imaging.
Eight years after Attariwala started scanning clients with his new MRI, he met Andrew Lacy, an Australian-born, California-based serial entrepreneur. Lacy was looking for his next venture and was interested in investing in the technology. He flew to Canada to undergo an MRI. The scan “told me more about my health than the health system had told me my entire life,” says Lacy. He was sold.
The pair went into partnership. Prenuvo moved its headquarters to California and focused on expanding south of the Canadian border, where markets are bigger and restrictions on private health facilities less complicated to navigate. The technology has improved since its first iterations two decades earlier, with higher image quality and speedier scans. Since then, more companies—including Ezra, Neko Health and simonONE—have joined the whole-body scanning market.
In 2022, Prenuvo opened its first clinic in Los Angeles. With it, the demographics of Prenuvo’s clientele suddenly changed. In Vancouver, the clients had an average age in the early 50s. Now, the clients were younger and into things like biohacking, an obsessive focus on making small changes to diet and lifestyle in order to improve health. Many L.A. clients also came with a sizable media presence. In 2022, American actress and television host Maria Menounos got a Prenuvo scan after months of undiagnosed pain, and it detected a mass on her pancreas, later diagnosed as a stage 2 pancreatic neuroendocrine tumour. In August 2023, Kim Kardashian posted on Instagram that she’d had a scan and wanted to tell her followers “all about this life saving machine.” Her post was not an ad, she wrote.
Lacy says the company did not plan to have an influencer-driven marketing strategy, but welcomed the online recommendations. Whole-body scans are a “completely new category of health care,” he says. “People aren’t googling for preventive health exams. Spreading word of mouth is the most important sort of activity we can do right now.” Prenuvo has offered complimentary scans to certain influencers in exchange for a review. The language used by social media celebrities as they talk about this technology often follows a pattern: They’re getting peace of mind. They’re taking preventative action. They’ll be coming back in future. They usually offer a code in their name for a US$300 discount.
More and more companies in the United States are now selling whole-body MRI scanning, although there are comparatively few in Canada. Prenuvo is the best known among the big players in the indus-try, with eight locations in the United States and another nine in the works. Currently, the company is working on adding a second scanner to its Van-couver clinic, doubling its Canadian capacity, and Prenuvo has plans to expand into Toronto, the U.K. and Australia in the future.
In Ontario, radiologists Nirav Patel and Keyur Shah opened Whole Body MRI in the fall of 2022. They now have locations in Mississauga and Ajax. They offer a 45-minute full-body MRI at $3,250, followed by an optional phone consultation with a radiologist. The pair would not say how many people have signed up for their MRIs, but say that the company is busy without having done much marketing. “We let it speak for itself, honestly. Doctors started coming in first, and then word of mouth. And it’s been growing and growing on its own,” says Patel. The demand is so high that some clinics have wait lists months long. When I checked at Prenuvo’s Vancouver clinic, the next available appointment was more than seven months away.
“I’d rather be safe than sorry,” explains Sarah Astles, 41, who is waiting to undergo her third scan in six years with Prenuvo. Astles used to work as an MRI tech and says she likes to be well-informed about her health; she notes that the scans reduce her anxiety. Her first scan results suggested she had “some kind of a bulge in my lower spine that [Prenuvo] said could be really debilitating.” She says the company encouraged her to return for a follow-up test. When she went back two years later, the bulge was gone. She says she was glad for the information even if the scan was costly and the results ambiguous.
“It was nice to know that, again, if I had major back pain, that’s probably what it was. And I could come back and check it in a year if need be. But if I went to the doctor with that kind of back pain without any other history, I’d probably be waiting a year for an MRI.”
She’s since recommended the screens to her mom and friends. She’d like to send her two children for scans when they’re older. The imaging allows her to feel like she’s not dependent on an overburdened Canadian health system, she says. “I just feel like in Alberta, in Canada in general, you really have to be your own advocate for anything.”
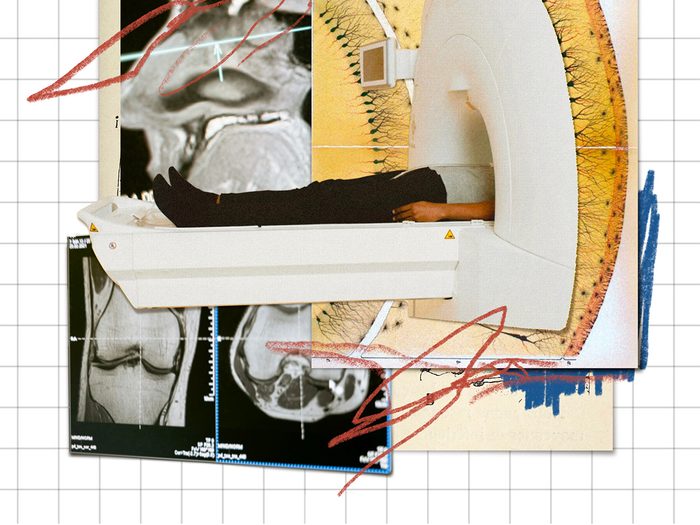
Whole-body MRIs performed on asymptomatic adults tend to pick up large numbers of incidentalomas, the term given to abnormalities detected unexpectedly on an imaging exam. Prenuvo says nearly all of us will have some imaging abnormalities. Some are life-changing, like a cancer diagnosis, and some are subtle things that might not ever make a difference to our health. Others are things to watch. Lacy argues that these findings inspire people to take better care of their health.
Prenuvo and other whole-body imaging companies do not provide the follow-up work to investigate what these abnormalities might be. That task falls primarily to family doctors and other health-care workers. That’s a problem, points out Braden Manns, a kidney doctor and health economist at the University of Calgary. He argues that improvements in modern imaging, along with more imaging being done, have driven up rates of overdiagnoses and incidentalomas. As a result, people are getting further testing, including invasive, potentially harmful procedures like biopsies that could lead to internal bleeding, and treatment for asymptomatic issues that previously would have gone unnoticed and may not have ever required treatment—some gallstones, damaged knees, bulging discs and blood clots, for example.
“It’s actually kind of scary for patients because if you’re well, they’re still going to find two to three abnormalities on the whole-body scans,” he says. “And then, of course, that leads to you going to see your doctor and that causes more stress.” Manns maintains that it’s more valuable for people to get reg-ular recommended evidence-based cancer screening like mammograms and colon cancer checks.
The follow-up investigations after a whole-body MRI also put patients at unnecessary risk for harm, adds David Urbach, a professor of surgery and faculty member of the Institute of Health Policy, Management and Evaluation at the University of Toronto. Whole-body MRIs can lead to more imag-ing, biopsies and surgery—which can cause pain, infection and even death. “In aggregate, [whole-body scanning] will harm your health,” he says.
It also hurts the Canadian healthcare system. Canada’s hospitals and medical clinics are already functioning beyond capacity. So are the people who work in them. The Canadian health system will struggle to manage the increased demand that arises from a growing industry of private-pay whole-body imaging, says Ania Kielar, president of the Canadian Association of Radiologists.
“When people have these types of tests that are done privately, and something is found, they often end up being further investigated within the public health-care system,” she says, “which adds increasing wait times for everybody else, costs to the system, and most of them are found to be benign.”
The current gush on social media for whole-body imaging rarely delves into the downside. It’s easier to convince someone of the potential benefits of screening than to educate them about the limitations, but this information should be presented to potential customers, says John Lysack, a professor of radiology at the University of Calgary. “As the saying goes, a half-truth is a whole lie. To have any chance of making proactive, informed decisions about their health, consumers would also need to understand the potential risks of whole-body MRI,” he says. “In a population of asymptomatic, otherwise-healthy individuals, findings on whole-body MRIs are much more likely to be benign incidentalomas than anything of clinical significance. The catch—and there’s always a catch—is that there’s no way on MRI, or on any other medical test, for that matter, to know with 100-percent confidence that any finding is entirely benign.”
Proponents and critics of whole-body MRI screening agree on one thing: Modern healthcare systems are designed to react to illness, not prevent it. There are limited supports available to help people keep disease at bay.
Lacy, at Prenuvo, says that when people see pictures of their insides, showing them bulging discs or inflammation in the liver, they’ll take preventive action. Manns, the health economist, urges people to do the same thing, but without the accompanying pictures: Take care of your health, he says. Eat properly, get regular recommended screening, exercise, practice good mental health care.
But as anyone who has lost someone to cancer knows, a healthy lifestyle isn’t always protective. For some people, the chance to know that something might be lurking underneath is worth the expense and the risk of potential harms. Milan Frydrysek puts himself in that group.
He hasn’t had an easy time since his diagnosis. After his surgery, he signed up for a medical study that put him on two medications that, it was hoped, would keep him cancer free. He suffered adverse side effects from the drugs, which severely damaged his thyroid and adrenal glands. Then, a regular follow-up scan in the public health system showed his cancer had returned. He now has stage 4 kidney cancer. He’s taking a new medication that has helped reduce the size of his tumours. He hasn’t gone back for a follow-up whole-body MRI; he gets regular scans as part of his cancer care now.
But he’d like his kids to have one. So far, they’ve said no.
Next: Women’s Health Collective Canada Is Addressing the Gap in Women’s Health
“On the trails, I slow down and de-stress,” says Shyrai Sutherland, a personal support and hospice worker living in Waterloo, Ont. She gets mental clarity by going outdoors for a hike, and it’s an important part of her overall wellness routine. As someone who juggles school (recreation and leisure studies at the University of Waterloo) and work, Sutherland says that hiking helps keep her physically fit and emotionally balanced. Sutherland isn’t the only one finding an eco-antidote to the stresses of modern life. Many therapists are recommending their clients get some “green exercise”—that is, a workout in the outdoors. Canadian doctors are also writing prescriptions: The PaRx program encourages people of all ages to head outside more often for increased energy, improved mood and reduced pain, stress and anxiety. Participants receive a nature “prescription” file and access to special offers from partners like Parks Canada and regional organizations like the Canadian Museum of Nature in Ontario.
Going outside can decrease your levels of cortisol, which lowers stress levels, says Sarah Kennell, the national director of public policy at the Canadian Mental Health Association. Kennell points to studies done on forest bathing (the practice of relaxing in a natural environment) that have found all sorts of benefits. “It’s an old and well-studied concept of getting out in nature and being present, removing headsets and devices and notifications and really taking a step back from day-to-day stresses,” she says. One recent study found that forest bathing reduces anxiety, depression, anger, mental fatigue and confusion while increasing vigour, which might indicate that it can help prevent depression. And the more time you spend outdoors, the greater the benefits. Kennell says that even 10 minutes hiking in nature would have “a significant positive impact on mental well-being, and extending the amount of time to 20 or 30 minutes would be an efficient stress reducer.”
Even without exercise or movement, simply engaging with the great outdoors has benefits. One study in Science found that patients who looked out a window while recovering from gallbladder surgery had decreased recovery time and asked for less pain medication. Where the benefits really kick in, though, is when you combine nature with exercise. “Research shows that about six weeks of moderate-intensity aerobic activity led to a decrease in severity of symptoms related to depression, anxiety and psychological distress,” says Kennell. “And if that exercise was taking place in nature, it could further boosts mental health impacts.”
Hiking has also been shown to reduce the risk of heart disease (thanks to the cardio workout it provides), lower blood pressure, build strong muscles and bones, improve arthritis and improve sleep. Hiking in nature can also help improve your balance: Hills, roots, sticks, mud and rocks all create an uneven terrain that challenges you to be steady on your feet. These physical benefits mean reaping mental health benefits as well, says Kennell. “There are positive correlations between increased aerobic activity and decreased cortisol levels, the hormone associated with stress,” she explains.
The nice thing about hiking is that it doesn’t really feel like exercise. Link up with a friend, bring your dog, experience new sights, sounds and smells—even the very same trail will change with the seasons. And the best part? All you need to get started is a bit of green space. Even parks within urban centres work great.

Get to know: Shyrai Sutherland
“I love the tranquility of being outdoors,” says hospice worker Shyrai Sutherland, “and just tuning into what I can hear, what I can see, what I can feel.” Sutherland fell in love with hiking in 2015, when she lived for 10 months near the Rocky Mountains in Alberta. Upon her return to Toronto, she kept it up.
In 2020, when the Black Lives Matter movement sparked a racial reckoning—especially as Christian Cooper was threatened and reported for “birding while Black”—Sutherland knew she had to act. She had watched people suffer mentally, socially and financially while many parks and leisure centres closed during pandemic lockdowns. She wanted Black people in her community to be able to gather, heal and enjoy outdoor spaces without fear. So she started Black Canadian Hikers. It’s a group dedicated to getting “other people who look like me out on the trails, taking up space and enjoying hiking and nature,” says Sutherland.
In May 2020, the first eight participants laced up their boots and hit a trail through Mono Cliffs Provincial Park in southern Ontario. “It was just so empowering and liberating,” says Sutherland. “I loved hearing feedback on how beautiful this experience was for people. How it opened up their worlds.”
Black Canadian Hikers meets monthly for guided hikes within the Toronto area and Kitchener-Waterloo. Some hikes have special add-ons, like guided meditations, yoga or birding. One focused on healing in nature for men. But the ultimate goal is relaxation, says Sutherland. “People are there to unwind; so, I just try to make it a positive experience.” —Valerie Howes
Next: The Awesome Health Benefits of Awe Walking
“In Japanese, it’s called ‘ukemi,’ which means ‘break fall,’” says Friba Rezayee, a judo athlete and former Olympian. She’s referring to the practice of learning how to use your arms and upper body strength to protect the rest of your body from impact with the ground. “Judo is a sport where you have to learn how to fall safely—so you fall but don’t get hurt.”
Ukemi might also be the perfect metaphor for Rezayee’s life and work with Afghan refugee women and girls. The 38-year-old gender equity leader and advocate is no stranger to setbacks. She was born and raised in Afghanistan, but when the Taliban came to power in 1996, she and her family were forced to flee to neighbouring Pakistan. When they returned in 2001, her political consciousness had been sparked. She enrolled at an all-girls high school and began learning judo at age 15, choosing the sport because of its combat nature and because martial arts were practiced indoors and in modest clothing.
“I’ve always believed, even as a child, that if you are born, you have the right to exist, to learn, to play sports,” she says. “I believe that human rights and women’s rights are innate, and we should have the right to practice and enjoy them.” In 2004, when Afghanistan was welcomed to the Summer Olympic Games in Ath-ens after being blacklisted during the Taliban regime, Rezayee made history at 18 as one of the first two female Olympic athletes from her home country. “My participation brought Afghanistan back into the world sports arena,” she says. “It was as if a door had been opened for the next generation of women and girls to play sports and participate.”
In 2011, Rezayee immigrated to Canada as a refugee, and a few years later she graduated with a bachelor’s degree in political science from the University of British Columbia. Her eyes and heart remained focused on Afghanistan, though, and in 2021 she incorporated her nonprofit, Women Leaders of Tomorrow, an organization dedicated to securing educational and sports opportunities for Afghan women and girls. “We advocate and work tirelessly,” she says of WLOT’s board, staff and volunteers. Since its inception, the organization has secured 20 scholarships for Afghan women and girls to come to Canada to study and has helped Afghan athletes further their education at home and abroad. Rezayee leads a busy life between her commitments to WLOT, her advocacy work and teaching judo to the next generation, but she’s driven by conviction: “Gender equity matters and that’s what leads me every day.”

BIG SHOTS Many of the women who come to Rezayee’s classes are interested in judo’s reputation as a combat and self-defence martial art. “Judo is a sport where you can learn how to lift someone up and throw them, even if they’re bigger and heavier than you,” she says. “Women really like that.”

GO STEADY Cross training for judo often means strength exercises, and Rezayee will head to the YMCA most days to weight-train at the gym or take a power yoga class. “I like the breathing style and stretches of power yoga. It helps me with balancing my body, and in judo you have to be able to balance well,” she explains.

KIDS STUFF Sundays are dedicated to sharing her knowledge of judo with the next generation. On Sunday mornings, she teaches two children’s classes at a local dojo, a highlight of her week: “It’s absolutely a joy and so fun to teach kids. We focus on techniques to help them move their bodies and minds together.”

TRUST THE PROCESS Rezayee demonstrates the bow, which begins and ends each judo exercise and is a symbol of respect. The objective of competitive judo is to throw an opponent, immobilize them or force them to submit using contact and impact. Partners are responsible for each other’s safety as they learn and progress.

TRICKS OF THE TRADE Alongside her teaching partner, Yuki Yokosawa—another former Olympian—Rezayee leads a drop-in judo class for women. Many of the attendees are beginners, but sometimes yellow-belt or even black-belt students join the class, and often Vancouver Police Department and RCMP members will attend.

WORK FOR HOME At some point during her day, Rezayee will hunker down on a judo mat for emails and phone calls. Since the Taliban’s return to power in August 2021, she’s fielded international media requests for comments on the situation in Afghanistan and her work with WLOT. “I try to make time for it all,” she says.

HEAVY MEDALS “Going to the Olympics was the best and worst thing that’s happened to me,” says Rezayee. “It was an honour and a privilege, but it came with its own risks and dangers. To be a pioneer of something is difficult. When you’re the first one, there is a lot of pressure on you. There are many barriers to overcome.”
Next: This Hockey Mom Will Motivate You to Get on the Rink
Liver—yes, even when it’s chopped—deserves far more respect than our culture doles out. The human liver performs upward of 500 functions: It filters our blood and regulates clotting, it’s the first line of defence against infection, it controls the balance of hormones and fats and it transforms our food into energy, and that’s just for starters. But its chief marvel lies in its power to regenerate—lop off a giant chunk of a healthy liver and the damn thing will grow back. Not part of the way. Not eventually. You can lose a whopping 70 percent of your liver and, only 12 weeks later, possess a full-sized replacement that behaves like brand new. No other organ in our body can do this. “That rapid regeneration is phenomenal, and the question is: How does it know when to stop?” says Sonya MacParland, the Canada research chair in liver immunobiology and a senior scientist at the Toronto General Hospital Research Institute. “If the liver constantly had this function, then you would be all liver. But somehow you don’t just blow up like a balloon.”
There’s plenty we don’t know about this organ. Why does scarring of the liver wreak havoc on our memory? Why does it secrete a hormone that might determine whether we have a sweet tooth? Why do female livers metabolize drugs more quickly, making women far more likely, regardless of age, weight or the amount of anesthesia given, to wake up during surgery? Here’s what we do know: The liver is roughly the size and shape of a slightly deflated football and sits in the upper right quadrant of our abdomen, just below the diaphragm. It weighs around three pounds, with a deep reddish-brown colour that comes from being positively saturated with blood—at any given moment, about 13 percent of our body’s supply.
Most of the liver’s 500-plus functions are performed by cells called hepatocytes. “They make up 80 percent of the cells in the liver,” MacParland says, “and they’re really the body’s workhorses.” Hepatocytes help the liver store iron, generate cholesterol and make the proteins that transport vitamins, enzymes and hormones throughout our bodies. They help produce the bile that whisks away waste and breaks down fats. They play a pivotal role in our immune system, helping to seek out and destroy invading bacteria and viruses. And they help store or release glucose, depending on the up-to-the-moment energy needs of our bodies and minds. “What’s unique about hepatocytes is their ability to perform many more functions than other cells in the body,” says Mamatha Bhat, a hepatologist and clinician scientist at the University Health Network’s Ajmera Transplant Centre.
But they are not, crucially, the only cells lurking in the liver. For decades, scientists studied the organ as a soup of cells, rather than as individual components—with predictably hepatocyte-heavy results. “Imagine a smoothie that is 80 percent banana,” MacParland says. “I can sneak in some avocado, maybe a bit of blueberry, and my kids will say it’s a lovely banana smoothie. That’s great for feeding my children, but not so great when we’re trying to figure out an organ.” And it’s those very small populations of less-detectable cells that, once dysregulated, can really drive disease.
So in 2018, MacParland and her colleagues created the first-ever map of the human liver, all the way down to the single-cell level. Using that detailed information, researchers can finally understand the different cell populations that make up a healthy liver, along with the ones that act out when things go wrong. And lots can go wrong in such a multitasking organ: There are more than 100 types of liver disease that together may affect 1 in 4 Canadian men, women and children. Non-alcoholic fatty liver disease is especially prominent, affecting 7 million people in Canada alone. Most experience no symptoms—you don’t tend to feel the damage to your liver until its functioning drops below 20 percent—but, left untreated, it can lead to cirrhosis and even cancer.
Still, there are reasons to be optimistic. Right now, transplantation may be the only option for patients with end-stage liver disease. But MacParland’s map can help inform more precise therapies, as researchers better understand how to reprogram the liver so patients don’t necessarily need a new organ. “The cool thing about certain subpopulations of cells is they’re actually very, very reprogrammable,” she says. “When we know how the cells are misbehaving, we can target therapies that reprogram those cells and get them to promote regeneration.” Bhat, meanwhile, works closely with computer scientists on algorithms to improve the trajectories of patients who do have transplants. AI tools can predict the individual risk of infection and disease for each patient, and personalize treatment and care to boost their long-term outcomes.
It’s a rare chance for tech to help a liver out. Mechanical ventilators can breathe for our lungs. Dialysis machines do the work of kidneys. Ventricular assist devices will pump for weakened hearts. “But it’s not actually possible to replace the liver with any machine,” Bhat says. “Its functions are just too complex.” So put some respect on the liver, chopped or otherwise—this organ is no superfluous side dish. It has main character energy that can’t be denied.
Growth Opportunity
During her residency in internal medicine, Mamatha Bhat, a scientist at the University Health Network’s Ajmera Transplant Centre and Toronto General Hospital Research Institute, sat in on a transplant for a patient with end-stage liver disease. Once the healthy organ was attached, the transformation was dramatic—and exceptionally fast. “I saw jaundice fully resolved within hours,” Bhat says. “The liver function just picked right up; it was quite amazing.”
At any given moment, hundreds of people are waiting on Canadian liver transplant lists. In 2022, according to data from the Canadian Blood Services, there were 520 people across British Columbia, Alberta, Ontario, Quebec and the Atlantic provinces. At least a quarter of them will die before they make it off the list. “Unfortunately, there remains an imbalance between the supply of organs and the need for them,” Bhat says. But remember that whole business about the liver’s remarkable power to regenerate—growing from 30 percent of its size back to normal volume in just 12 weeks. We leverage that rapid liver regeneration in our program, which is the largest living donor liver transplant program in Canada, to save the lives of people on that list,” she says.
If you’re between the ages of 16 and 60 and in good health, you could help with this life-saving work. Living donation is not minor surgery: The operation lasts about six to eight hours, removes at least half of your liver (usually the entire right lobe) and requires a five- to 10-day stint in the hospital. Full recovery will take another six to eight weeks, though your organ will function like normal right after the surgery. As for that donated liver, it’ll be matched with a patient on the transplant list based on compatible size and blood type. But here’s a wild fact: You can put a liver that’s a little too large into someone who’s a bit smaller, and the liver will actually shrink to fit.
“Out of the more than 200 liver transplants we perform in our program each year, 70 to 80 percent are from living donors, and there’s even a certain percentage that are from anonymous living donors,” Bhat says. “It’s beyond being a good samaritan. It’s just a completely selfless act.”
The Sweet Spot
When you last went to the movies, did you settle in with a bucket of popcorn? Or did you chase gummy bears with M&Ms instead? After running the bloodwork on more than 6,500 Danish participants, researchers at the University of Copenhagen found a link between a liver-secreted hormone called fibroblast growth factor 21 (FGF21) and people’s appetite for sugary treats.
FGF21 seems to act like a candy-coloured stop sign. When researchers measured its levels in study participants who’d fasted for 12 hours, they discovered that sweets-scorning Danes had 50 percent more FGF21 in their systems than those who confessed to a serious sweet tooth. And the composition of the gene matters, too. Some participants had particular—and apparently weakened—variations of FGF21. Those folks were much more likely to eat larger amounts of gummies and sweets.
What does it mean? Like much that has to do with the liver, it’s an ongoing question. But the results suggest that our livers do send out signals about the foods and nutrients that we need. And now, when you find yourself forgoing the chips for a Hershey bar, you know which organ to blame.

Snooze Patrol
The brain gets all the credit for serving as our master biological clock: It’s the circuitry that governs our circadian rhythms, the 24-hour cycle dictating everything from our appetite and body temperature to our sleepiness, immune system and mental health. But what if—you guessed it—the liver had something to do with these rhythms as well? Euro-pean researchers set out to see if they could make the connection.
Back in 2017, working with mice, which also run on a 24-hour clock—the researchers were amazed to find that livers grow and contract by more than 40 percent over the course of the day. Because mice are nocturnal, eating by night and dozing during the day, the size of their livers nearly doubles after dark. It makes sense: Liver cells need to work hard to convert food into fuel, so they swell to ensure peak production. But once it’s bedtime, there isn’t the same need for that effort, so the liver powers down to conserve energy.
Here’s the catch. When researchers messed with the mice’s circadian rhythms, forcing them to stay awake and feed during the day instead of at night, their livers didn’t undergo the same growth and contraction, even if the mice were eating the same amount. It suggests that the cues that spur our livers into action don’t come from our food—they come from the biorhythm that’s evolved in us over hundreds of millions of years.
So what happens when mice are wound up using a different clock altogether? Last year, some of the same European researchers returned for another experiment. This time, they switched out the liver cells in the mice with human liver cells, and, all of a sudden, the mice started to look a lot less nocturnal. Their daily cycle moved forward, and they began to eat and be active a full two hours before nightfall.
These twin studies underscore the intimate relationship between our liver and our biological clock. And that’s important, because all sorts of modern interventions, including night-shift work, jet lag and the blue light of our laptops and phones, conspire to throw that innate sense of time out of whack. It’s clear already that night-shift work, for example, carries the risk of all sorts of adverse health effects, including cardiovascular disease, diabetes and cancer. The researchers suspect that deregulation of our biological rhythms also has significant consequences for the functions of our liver—and, as we know, the liver controls an awful lot.
Next: How Heart Disease Affects Women Differently Than Men
Before there was tiramisu, carrot cake occupied the top spot in my dessert hall of fame. And of course, I have opinions about it. The cake should be moist, with a very tender crumb, and packed with carrots. I don’t love nuts and raisins, but I can respect them, so you’ve got the option to add them here. And always cream cheese icing. Since the flavour of store-bought vegan cream cheese varies widely, I have created a cream cheese–inspired cashew frosting.
Carrot Cake with Cashew Frosting
Makes one 2-layer round cake
Ingredients
Cashew Frosting
- 1 cup (250 mL) cashews, soaked in boiling water for 30 minutes and drained
- ½ cup (125 mL) canned full-fat coconut milk
- 3 tablespoons (45 mL) pure maple syrup
- 2 tablespoons (30 mL) freshly squeezed lemon juice
- 2 tablespoons (30 mL) coconut oil
- 1 teaspoon (5 mL) pure vanilla extract
- ⅛ teaspoon (0.5 mL) salt
Carrot Cake
- 1½ cups (375 mL) almond flour
- 1½ cups (375 mL) gluten-free flour blend
- 2 teaspoons (10 mL) baking powder
- 2 teaspoons (10 mL) cinnamon
- 1 teaspoon (5 mL) baking soda
- ½ teaspoon (2 mL) salt
- 2 cups (500 mL) firmly packed grated carrots (about 2 large carrots)
- 1 cup (250 mL) unsweetened applesauce
- ½ cup (125 mL) extra-virgin olive or avocado oil
- ¾ cup (175 mL) cane sugar
- ½ cup (125 mL) unsweetened oat milk
- ¼ cup (60 mL) ground flaxseed
- 1 tablespoon (15 mL) apple cider vinegar
- 1 teaspoon (5 mL) pure vanilla extract
- 1 teaspoon (5 mL) grated peeled fresh ginger
- ½ cup (125 mL) raw pecans or walnuts, chopped (optional)
- ½ cup (125 mL) raisins (any type; optional)
Directions
- Make the cashew frosting: In a high-speed blender, com- bine the drained cashews, coconut milk, maple syrup, lemon juice, coconut oil, vanilla, and salt. Blend on low speed, then slowly increase to medium-high until smooth, 1 minute. Scrape the frosting into an airtight container and transfer to the fridge to firm up for at least 1 hour before using. The frosting can be stored in the fridge for up to 4 days.
- Meanwhile, make the carrot cake: Preheat the oven to 350°F (180°C). Lightly grease two 8-inch (1.2 L) round cake pans with butter or coconut oil and line with rounds of parchment paper to fit the bottom of the pans for easier removal.
- In a large bowl, stir together the almond flour, gluten- free flour blend, baking powder, cinnamon, baking soda, and salt.
- In a medium bowl, mix together the carrots, applesauce, olive oil, sugar, oat milk, flaxseed, apple cider vinegar, vanilla, and ginger. Add the wet ingredients to the dry ingredients and stir to combine. Fold in the nuts and raisins, if using.
- Scrape the batter into the prepared cake pans. Bake until the tops are firm and dry to the touch, the cakes are golden brown around the edges, and a skewer inserted into the centre of the cakes comes out clean, 33 to 37 minutes. Remove from the oven and let cool in the pans for 10 minutes, then carefully (the cakes will be soft) invert the cakes onto a rack and cool completely. Unfrosted cake layers can be stored, tightly wrapped, on the counter for up to 2 days.
- Assemble the cake: Remove the cashew frosting from the fridge.
- Place 1 cake layer top side up on a cake plate. Using an offset spatula, spread one third of the frosting over the cake layer to the edge.
- Carefully set the second cake layer bottom side up on top of the frosted layer and spread one third of the frosting over it. Use the remaining frosting to frost the sides. Store the frosted cake, covered, in the fridge for up to 4 days. (Once the cake is iced, it must be kept refrigerated until ready to serve or the frosting will melt.)
Excerpted from Plant Magic by Desiree Nielsen. Copyright © 2024 Desiree Nielsen. Published by Penguin, an imprint of Penguin Canada, a division of Penguin Random House Canada Limited. Reproduced by arrangement with the Publisher. All rights reserved.
Next: Need a New Go-To Lunch Recipe? Try These Soba Noodles With Miso Pecan Butter
We’ve turned just about every facet of our health into data—our steps, our resting heart rate, the instant we ovulate—so it’s no surprise we’re starting to gamify our orgasms. A growing number of smart sex toys can chart the intensity of those orgasms and provide titillating data on how often and how well we come.
Take, for example, the Lioness. This vibrator has built-in sensors that measure tension (which reflects arousal and how close you are to finishing), temperature (to track when it’s inside you) and motion (to follow how you’re moving the toy). The data captured is sent to an app that maps each session, showing vaginal contractions as a spike. The stronger the contraction (and thus the pleasure), the higher the spike. Newer models of the Lioness even let you see real-time data on your phone as you’re self-pleasuring. With all that info, you can start to figure out what actions get you off the most. And while it can definitely help people who struggle to know what they like, turning self-pleasure into a numbers game—and trying to score new personal bests—might not be so great for our relationship with our orgasms.
These toys tap into one of the foundational myths of women’s health: that our orgasms need to be better. That myth causes people to constantly search for ways to improve their orgasms, and women’s media, in response, publishes all sorts of reassurances that good orgasms are possible. Some articles offer science-backed tips. Others recommend breathing tricks. Some tell you how to have multiple orgasms each time, or how to have a squirting orgasms (which, full disclosure, has been Best Health’s most-read article online for years).
But thanks to William Masters and Virginia Johnson, we’ve known since the 1960s that women are just as capable as men of reaching orgasm—if not more capable. Those researchers mapped out what happens to the body during sex, and, among their discoveries, they found that women don’t experience a refractory period, which means they’re capable of more orgasms—multiple, successive orgasms. Men, meanwhile, can’t get aroused for anywhere from minutes to hours after ejaculation.
“Every study since Masters and Johnson has found that if there is any difference between male physiology and female physiology, it’s that females have a greater capacity for orgasms,” says Tina Fetner, a professor of sociology at McMaster University and author of Sex in Canada: The Who, Why, When, and How of Getting Down Up North. Fetner’s book breaks down the results of a comprehensive, first-of-its-kind coast-to-coast study looking at the sexual activity of average Canadians. Social differences, she found, affect sexual behaviour: Older women, for example, are less afraid to ask their partners for pleasure than their younger counterparts, while francophones have more sex altogether.
So how did we get here? In no small part, unsurprisingly, it’s the patriarchy. The primacy of the male orgasm has led to an idea of sex and pleasure that screws us all: Both partners in a heterosexual relationship work toward the male orgasm, so women’s orgasms are seen as a “side effect of the kind of activity that brings men sexual pleasure,” says Fetner. Penis-in-vagina sex is great at making men come, but most women need clitoral stimulation to get off. And when a woman can’t come after male-focused sex, it’s seen as a problem—when it’s seen at all.
There’s a lot of pressure, then, on women to achieve orgasm (even that turn of phrase—achieve). And there isn’t necessarily a simple answer, although stimulating the clitoris generally helps, especially through oral sex and foreplay—though these acts can be seen as special, not routine, Fetner says. According to her findings, men who identify as feminist and prioritize their partner’s pleasure are more likely to engage in clitoris-stimulating acts like oral sex.
At the end of the day, a happy ending is whatever you want it to be. That might look like optimizing your orgasm: “If you want to gamify sex, or outscore yourself every time, well, who am I to deny anyone access to sexual pleasure?” Fetner says. It could mean moving oral sex from “extracurricular” to “must-do” or introducing a stimulating lubricant to increase the sensitivity of your clitoris. What it doesn’t look like is disciplining your body to perform in a certain way. Says Fetner: “That just makes it more and more difficult to be in your body—and enjoy what you enjoy.”
Next: Your Showers Are About to Get a Lot Longer (But Not for the Reason You Think)