The “Other” Virus That’s Putting Those 50+ at Risk
One in three adults over 50 will develop shingles, a painful virus caused by varicella zoster. Here's what you need to know to protect yourself.
For Françoise Fontaine, acne was but a long-ago memory of adolescence. Yet there it was, unmistakable, little red bumps in a straight line across the Paris resident’s forehead that a friend noticed after a day of shopping.
It must be an allergic reaction to the clothes I just bought, she thought. But just in case, Fontaine called her long-time doctor the moment she got back home and described her symptoms.
“I think I know what you have,” the doctor told her. “There is no need to panic. My assistant will bring you anti-viral medication, which you should take right away and go see an eye specialist as soon as possible.”
The next morning, Fontaine was sitting in the specialist’s office, shocked as he informed her she had a virus called shingles, also called herpes zoster.
“It occurs when a virus called varicella zoster, which causes chicken pox, reactivates,” he explained. “You had chicken pox as a child, no?”
She had. But she didn’t know the virus that caused it had been lurking in the nerve endings of her spinal cord ever since, dormant, waiting to catch her immune system off guard before pouncing again. Or, that for some patients while the rashes and blisters fade, the tingling and burning from what is called post-herpetic neuralgia, or nerve damage, can last with little respite.
That was almost a decade ago. Now Fontaine, says: “I was lucky. The outbreak didn’t affect my eyes. But no matter what I try, the pain persists to this day. In that way, I guess I’m not so lucky.”
Most shingles outbreaks last no more than a week or two but some patients are at greater risk of developing life-threatening complications, including those who are undergoing treatment for cancer.
Research released back in 2015 found that a severe case of shingles can raise the risk for stroke and heart attack — and kill. Caroline Minassian, PhD, and colleagues from the London School of Hygiene and Tropical Medicine in England looked at the records of more than 67,000 US Medicare patients who had shingles and suffered either a stroke or a heart attack within a year.
“We observed a 2.4-fold increase in the ischemic stroke rate and a 1.7-fold increase heart attack rate,” researchers reported in the Public Library of Science Journal. “The most marked increase was observed during the first week following zoster [shingles] diagnosis.”
Researchers suggested two possible reasons: the virus causes fatty build-ups in the arteries to break off and cause a stroke or a heart attack, or the stress caused by the pain sends blood pressure up, again resulting in a stroke or a heart attack.
Further research into shingles at the Mayo Clinic in Minnesota also showed that adults with asthma appeared to have a 70 percent higher risk of developing shingles, compared with those without asthma.
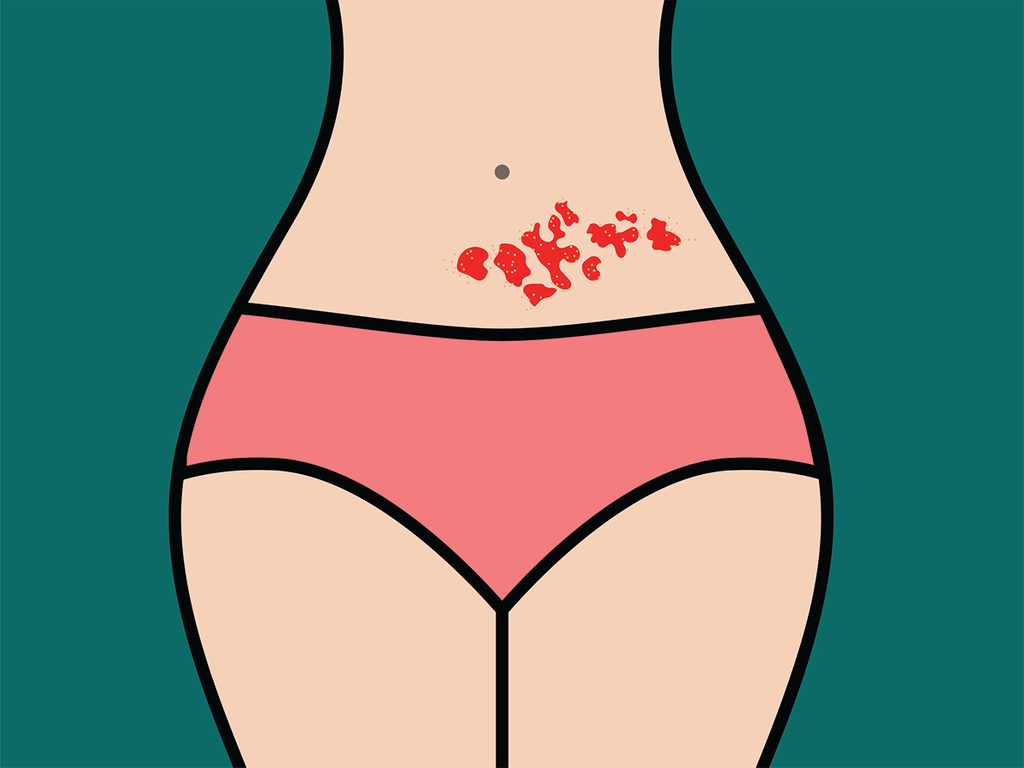
There is no cure for shingles. Its name that comes from the Latin and French words for “belt” because it often appears at waist level, partly circling the body. Dr. Allison Mc Geer, a microbiologist at Toronto’s Mount Sinai Hospital, enumerates the symptoms, which tend to occur on one side of the body because only a single nerve root is usually involved.
These may include numbness or tingling, itching and fatigue, headaches, high fever, a sensitivity to light and excruciating nerve pain that can upend your life, leaving you sleepless, unable to work or carry out daily activities.
“As you get older, your immune system stops paying attention to the virus for a period of time so that it grows down the nerve root, unimpeded.” Dr. Alison McGeer paying attention to the virus for a period of time so that it grows down the nerve root, unimpeded,” Dr. McGeer explains. “The resulting skin rashes have distinctive shapes because they follow the pattern of the nerves as they give feeling to our skin.”
Unlike chicken pox, shingles is not contagious. If you are exposed to someone with shingles, you will not get the virus as long as you have had chicken pox, Dr. McGeer says. However, if you’ve never had chicken pox and are exposed to someone with shingles, you may come down with the childhood disease.
Timo Vesikari, a professor of virology at the University of Tampere in Finland, and director of the institution’s vaccine research centre, says most people will have only one shingles outbreak in their lifetime because it serves as a reminder for the immune system to become vigilant again. Still, depending on how old you are when the first outbreak occurs, it is possible to have a second one and maybe even a third. With life expectancies in Europe and North America longer than ever before, and with the baby boomer generation well into shingles territory, physicians are girding themselves to see more cases than ever before. Says Vesikari: “Think of it this way — if we all lived for 200 years, then everyone would develop shingles at some point.” Given that one in three adults over the age of 50 will develop the disease, it is best to prevent an outbreak in the first place. “For this you have to get a vaccine,” says Vesikari. If you’ve not been vaccinated, then you need to act quickly, at the first sign of symptoms, as the anti-viral medication is best used within 72 hours of an outbreak. This is especially important if you are hoping to mitigate the very painful post-infection pain that can often occur.
Currently, there are two vaccines, according to Health Canada. The first, Zostavax, was approved for use about 14 years ago and reduced the chance of an outbreak by 64 percent. But with ingredients such as live chicken pox virus, it was difficult to produce in large quantities and, thus, expensive. As for efficacy, experts believed it only offered immunity for about five years.
The newer vaccine is called Shingrix, and is the one Health Canada recommends for people aged 50. Unlike Zostavax, Shingrix does not contain any live virus, instead combines an easily replicated protein found in the virus with an adjuvant, or chemical substance, that helps the body’s immune system wake up. Adjuvants are already used in vaccines to prevent a host of conditions, including hepatitis A and B, diphtheria and tetanus, but this is the first time one has been used in the battle against shingles. Shingrix is generally thought to be more effective and longer lasting.
As always, speak with your healthcare provider for the best fit for you as previous history needs to be taken into account.
If you have not been vaccinated, learn to recognize the early signs of shingles and call your doctor as soon as you suspect something’s wrong.
Vancouver resident Marilee Sigal wishes she had done just that when she had a shingles outbreak three years ago. Just turned 55 at the time, she was sitting with guests in her back garden on an evening in August, 2013, when she felt a sharp pain high on the left side of her back. At first, she attributed it to fallout from a fierce childhood battle with scoliosis, a sideways curvature of the spine.
But the pain didn’t subside. It got worse. A day later Sigal noticed a mark like an insect bite. Finally, another day after that, she went to a walk-in clinic. There the doctor looked at it and said, “I can wait for test results, but I’ll tell you right now that it’s shingles.” Sigal, now 62, was surprised. As a psychotherapist, she kept up on medical literature and thought she would be at risk only when she reached 60.
The doctor prescribed antiviral medication but it was too late because Sigal had experienced the first symptoms more than three days earlier.
For Françoise Fontaine, the journey has been difficult. She has tried all kinds of therapies, from acupuncture to hypnosis to stop the burning pain. But nothing has worked. “I have to protect my skin from the sun and the wind because it hurts,” she says. “Some nights, it is just awful. I can’t sleep and I scratch myself until I bleed.” Still, she goes on one day at a time, spirited and determined to live each one to the fullest.
Next, learn the health secrets every woman over 50 needs to know.




