Women’s College Hospital Among First to Offer Health Records on iPhone
Dr. Danielle Martin explains who could benefit most from Apple Health Records's launch in Canada.
Toronto’s Women’s College Hospital took another big step in its virtual care strategy yesterday, with the announcement that it’s one of three institutions in Canada to now offer Apple’s “Health Records” feature to patients with iPhones.
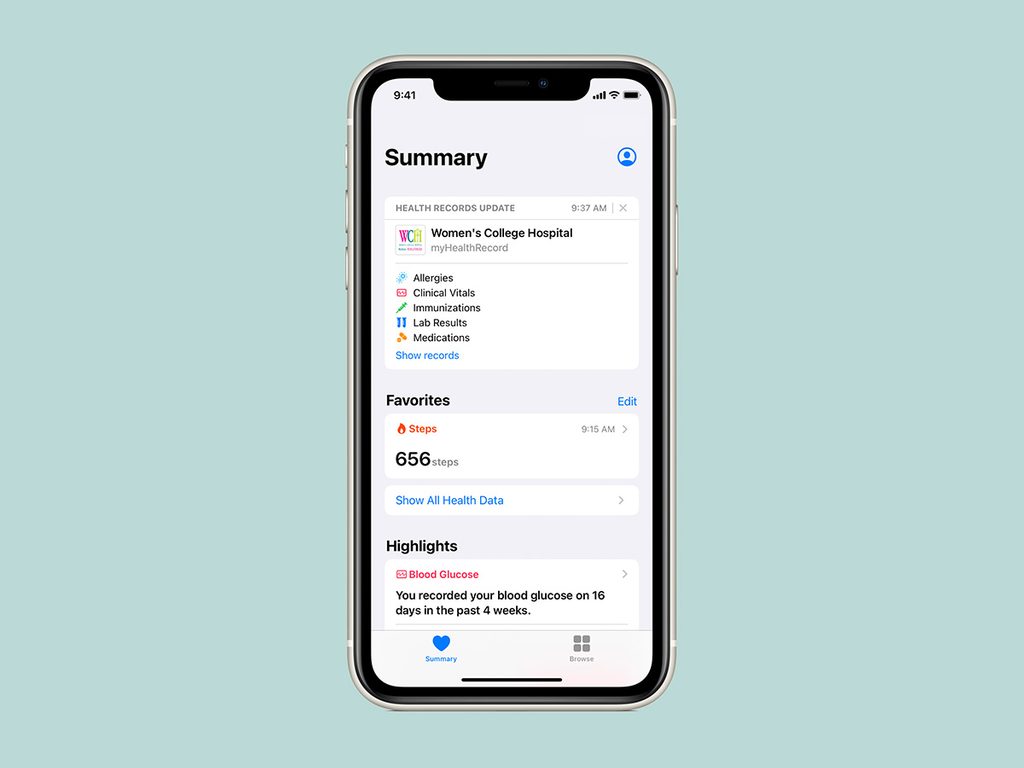
Health Records, which lives within Apple’s Health app, allows people to receive and store medical records from connected hospitals directly on their device — everything from their allergies and immunizations to lab results and pathology reports. It can also alert you when new reports or results arrive.
The feature, which is currently active in the U.S., aims to empower patients by providing easy, consolidated access to information from multiple healthcare providers at all times. St. Joseph’s Healthcare Hamilton and Mackenzie Health in Richmond Hill, ON, are also rolling out the feature to their patients, said Kevin Lynch, Apple’s vice-president of technology. He added he hopes more institutions across Canada will now come on board (more than 500 health systems offer the feature in the U.S.).
(Related: Why You Should Be Tracking Your Menstrual Cycle)
In terms of security, Lynch said privacy was considered from the ground up when developing the feature. He explained that the reports flow into the app via a direct encrypted connection between your device and your hospital’s online patient portal — once the reports are downloaded, they are secure, private and encrypted on your device. If you choose to back up the information in iCloud, it’s encrypted in transit and at rest as well. The data is never accessible by Apple, or shared with third-party apps without explicit permission from the individual, Lynch said.
Danielle Martin, executive vice president and chief medical executive at WCH, spoke to us about why her hospital was keen to be an early adopter of this initiative, the potential benefits to patients, and how WCH is tackling issues of equity and accessibility.
(Related: Apple Watch ECG is Finally Available in Canada)
Why is virtual health care a priority for WCH?
Health care is a human business and we will always deliver face-to-face care at WCH, but if we ask someone to come on the subway, or drive here and park for $24, and wait in a waiting room for 45 minutes to see a healthcare provider, it should be because that’s the best way to deal with their issue — not because it’s the only option. We launched Women’s Virtual, Canada’s first virtual hospital, in 2018, and have been rolling out a variety of programs and approaches that are intended to increase options for people in getting access to care.
How does Health Records fit into that plan?
Part of our commitment is that we believe that people should have access to their own records, and we believe that the integration of information from many different sources should happen, ideally, at the level of the patient.
We’ve made choices in Canada about electronic medical records over many decades that have resulted in systems that don’t talk to each other. I think it’s highly unlikely that’s going to change. But there’s no reason why, in this day and age, it has to, because all of the data integration can occur at the level of the patient. That’s why we’re excited to implement Apple Health Records.
It’s not for everyone. And it’s not going to fix everything. But a lot of Canadians have an iPhone, and as more organizations sign on, people will be able to access their data from all over the healthcare system, in the palm of their hand.
What would you say to someone who’s concerned about privacy?
We did a lot of due diligence to make sure this meets all privacy and security requirements. An important feature from our perspective is that the information flow is one way. We have a secure patient portal right now — a patient can sign up and access things like blood test results, imaging results and pathology results. We’ll be increasing what’s available through that portal over time. But with Apple Health Records, when a patient clicks the ‘I agree’ button, now the information flows not just into the portal but into the Health Record app on their phone. And it’s closed only to them. There’s nothing coming back to us.
Who will benefit most from this?
In my view, the people who really stand to benefit from this are those with multiple, complex, chronic illnesses, whose care is managed in different places all over the system. I have lots of patients like this. They might see a cardiologist at one hospital and an endocrinologist at another, and then have to go to an emergency department somewhere closer to home. The management of keeping track of all of those appointments and what tests have been done, and communicating all of that to multiple doctors — it’s a lot of energy and a lot of work. So to me, this feature will be most useful if healthcare organizations all over the province and country sign up. That’s when it will be truly, clinically useful.
What are the roadblocks that come with this kind of virtual care?
We always worry about the digital divide. We want to make sure that these kinds of advances don’t leave a bigger gap between those who have access to this kind of technology and those who don’t.
We work really hard to find ways to serve people who don’t have easy access to technology, and never make assumptions about who has a phone and who doesn’t. I think the best that we can do is to be consciously attending to the equity dimension in virtual care writ large, and that doesn’t just apply to Apple Health Records. It applies to everything we do.”
What’s next for WCH in its work on the health gap?
We’ve been doing a lot of work during the pandemic on equity analysis, and striving to develop programs designed for vulnerable or underserved groups that makes accessing healthcare easier more convenient than having to take a half day off work and coming to a hospital. Our next big push is going to be in the area of surgery. We are aspiring to be a place people come to in person, only if there’s something that needs to be done in person. And so we’re looking at how to do preoperative care and post-operative care through a variety of access a virtual means.
We’re also accelerating our strategy for what we call ‘aging-in-place.’ One of the things the pentamic has shown us is how vulnerable seniors are in long-term care. And we know there are many more seniors living in apartments or retirement homes who are experiencing isolation and loneliness. So we’re thinking about how to design virtual care services that are meaningful and helpful to connect seniors, so they can age in the place where they want to age.
Of course, there are lots of ways to connect with people that don’t require broadband or a fancy laptop. There’s this thing we call ‘the phone’ that works really well for a lot of things. We are interested in exploring the full spectrum of virtual care, including the low-tech version.
Next: ‘I Have a Cloud Over Me’: How Isolation Affects Seniors Living at Home




